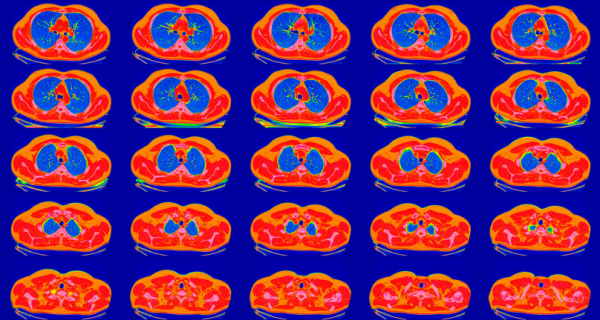
New guidelines aim to screen millions more for lung cancer
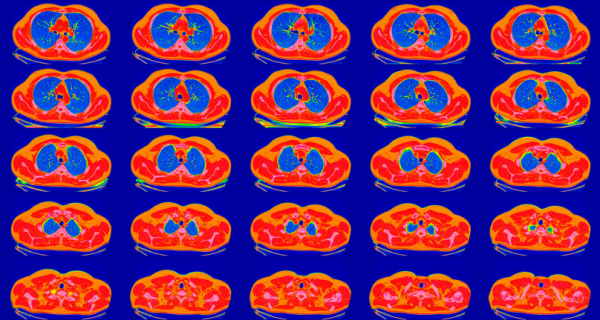
Lung cancer kills more Americans than any other malignancy. The latest American Cancer Society (ACS) updated guidelines aim to reduce deaths by considerably expanding the pool of people who seek annual, low-dose CT lung screening scans.
Advocates hope the new advice will prompt more people at risk for lung cancer to schedule yearly screening, says Dr. Carey Thomson, director of the Multidisciplinary Thoracic Oncology and Lung Cancer Screening Program at Harvard-affiliated Mount Auburn Hospital, and chair of the Early Detection Task Group for the ACS/National Lung Cancer Roundtable. Currently, fewer than one in 10 eligible people in the US follow through on recommended lung screenings.
What are the major changes in the new ACS lung cancer guidelines?
The updated ACS guidelines are aimed at high-risk individuals, all of whom have a smoking history. And unlike previous ACS recommendations, it doesn’t matter how long ago a person quit smoking. The updated guidelines also lower the bar on amount of smoking and widen the age window to seek screening, which aligns with 2021 recommendations issued by the US Preventive Services Task Force.
These changes combined may mean another six to eight million people will be eligible to have screening.
How many people get lung cancer?
Although lung cancer is the third most common malignancy in the United States, it’s the deadliest, killing more people than colorectal, breast, prostate, and cervical cancers combined. In 2023, about 238,000 Americans will be diagnosed with lung cancer and 127,000 will die of it, according to ACS estimates.
What is the major risk factor for lung cancer?
While people who have never smoked can get lung cancer, smoking and exposure to secondhand smoke is a major risk factor for this illness. Smoking is linked to as many as 80% to 90% of lung cancer deaths, according to the CDC.
Indeed, people who smoke are 15 to 30 times more likely to develop or die from lung cancer than those who don’t. The longer someone smokes and the more cigarettes they smoke each day, the higher their risks.
Is lung cancer easier to treat if found in early stages?
Yes. As with many cancers, detecting lung malignancies in their earliest stages is pivotal to improving survival.
Depending on the type of lung cancer diagnosed, up to 80% to 90% of people with a single, early-stage tumor that can be removed surgically can survive five years or longer, says the American Society of Clinical Oncology. The number of people who survive long-term becomes smaller as tumors grow larger, and if they spread to lymph nodes or other areas of the body.
Should you consider lung CT screening?
The updated ACS guidelines recommend screening if you:
- Are 50 to 80 years old. This age range is expanded from the prior ACS recommended cutoff of 55 to 74.
- Are a current or previous smoker. This includes anyone who smoked, not just smokers who quit within the past 15 years.
- Smoked 20 or more pack-years. This means smoking an average of 20 cigarettes per day for 20 years or 40 cigarettes per day for 10 years. Previously, the eligibility cutoff was 30 or more pack-years.
“While an expansion in the number of people screened for lung cancer will find additional early tumors, it also means more false positives will be detected,” says Howard LeWine, MD, Chief Medical Editor at Harvard Health Publishing. False positives are worrisome spots on a CT scan that are not cancer. But they usually require additional testing, perhaps a biopsy and even surgery for something that was harmless.
Before scheduling a low-dose CT lung screening, you’ll need to talk to a health professional about the screening process, your risks, whether it will be covered by your health insurance. Previously, an in-person medical appointment was required.
Why did the ACS change the years-since-quitting screening requirement?
Much international research suggests that the number of years since someone stopped smoking has little or no bearing on their risk of developing lung cancer, says Dr. Thomson.
“You have an equal likelihood of developing lung cancer whether you quit more than 15 years ago or more recently,” she says. “The recommendations on the national scene say that we need to be screening more people and make it easier to be screened. One of the ways to do that is to drop the quit history requirement.”
If you’re eligible for screening, how often should you have it?
Every year, says the ACS.
But why not screen for lung cancer for several years and then take a break, as is done with a malignancy such as cervical cancer? Research hasn’t been done to demonstrate that this type of approach is safe, Dr. Thomson says.
“We know that a large percentage of lung cancers identified in people through low-dose CT scans are identified after their first year of screening,” she says. “And some forms of lung cancer can move quickly, which is part of the reason it’s as deadly as it is.”
Did all guidelines organizations drop the years-since-quitting requirement?
No. The Centers for Medicare & Medicaid Services (CMS) and the U.S. Preventive Services Task Force — which, along with the ACS and other groups, recommend national standards for screenings — haven’t yet signed on to the ACS approach. These two groups maintain that only smokers who quit 15 or fewer years ago should remain eligible for screening.
However, guidelines issued by the National Comprehensive Cancer Network mesh with the new ACS recommendations by not having a years-since-quitting threshold.
Because Medicare and other health insurers may have slightly different rules to determine payment for lung cancer CT screening, it’s best to confirm this with your health care provider or insurer before getting tested.
About the Author

Maureen Salamon, Executive Editor, Harvard Women's Health Watch
Maureen Salamon is executive editor of Harvard Women’s Health Watch. She began her career as a newspaper reporter and later covered health and medicine for a wide variety of websites, magazines, and hospitals. Her work has … See Full Bio View all posts by Maureen Salamon
About the Reviewer
Howard E. LeWine, MD, Chief Medical Editor, Harvard Health Publishing
Dr. Howard LeWine is a practicing internist at Brigham and Women’s Hospital in Boston, Chief Medical Editor at Harvard Health Publishing, and editor in chief of Harvard Men’s Health Watch. See Full Bio View all posts by Howard E. LeWine, MD